Experimental drug may one day save thousands of accident victims
Photo courtesy of Harborview Medical Center
Somewhere on a wet rural road in Western Washington, fate decrees disaster: A logging truck fails to negotiate a sharp, blind curve. It skids into the path of an oncoming passenger car. Tires squeal as drivers attempt, in vain, to prevent the inevitable.
Minutes later another truck comes along. Rounding the same blind curve, its driver confronts a grisly, smoking scene of chaos and destruction. He stops and radios for help.
Almost instantaneously, Washington’s highly sophisticated emergency response units kick into motion. Medical personnel speed to the scene of the accident—a confused mass of flipped and flung machinery.
When paramedics arrive, they discover that the car’s teen-age driver—the only survivor—is in deep shock and suffering from extensive injuries that include an almost completely severed hand. They radio Airlift Northwest, the region’s air ambulance service, to dispatch a specially equipped helicopter to the site.
Sixty miles away, at Harborview Medical Center’s Regional Trauma Center in Seattle, hospital staff prepare to receive the casualty—something they do, on average, 20 times a day. When the patient arrives, he is quickly transferred to surgery. Over the next 10 hours, an eight-member surgical team—including physicians, nurses and technologists—painstakingly repairs the youth’s major injuries. They close the wounds, stop the bleeding, and reattach the partially severed hand. With transfusions, blood pressure returns to normal.
Now out of surgery, the young man’s prognosis at first looks good. But his condition takes a sudden, dramatic turn for the worse: His body begins to swell noticeably. Vital signs weaken one by one as heart, liver, kidneys and other organs begin to fail.
Before their eyes, family members, physicians and nurses watch helplessly as a rapidly plummeting cascade of events threatens to cancel every good thing done to help save this teenager since his accident. In a few hours, his own body’s reaction to the trauma takes his life.
* * *
This story is fictional, but real ones like it happen every day throughout the nation. To people like Dr. Charles Rice, the situation is all too familiar.
“The trauma surgeon often is able to stop the bleeding and repair damaged tissues, only to have the consequences of shock set off an inflammatory cascade that undoes this handiwork,” says Rice, professor of surgery at the UW School of Medicine and surgeon-in-chief at Harborview Medical Center (one of two UW teaching hospitals).
What killed this hypothetical trauma victim is a product of shock called multiple organ failure syndrome. The deadly condition is believed responsible for killing almost half of the 50,000 trauma victims who develop it each year in the United States, often despite some of the best medical attention available anywhere in the world. At Harborview alone, nearly 400 patients with this syndrome are seen annually. And this deadly condition does not strike only trauma victims. Patients with massive infections also suffer—and die—from multiple organ failure.
Years ago, multiple organ failure was not a major concern, since victims of severe trauma rarely survived. But now, with the advance of surgical techniques, trauma surgery teams can repair the physical damage, only to see their patients die anyway.
Ironically, it is advanced medical care itself that may offer a cure for multiple organ failure syndrome and related conditions. New technologies and drugs provide unprecedented chances for saving lives that have caught nature—and evolution—unprepared to cooperate with each other in the body’s fight for survival.
One potential drug developed by UW researchers could possibly have saved our accident victim. It goes by the distinctly unglamorous name of MAb 60.3 (in informal moments some have called it “the juice”) and it’s part of an increasingly promising area of medical research called antiadhesive therapy.
Among the UW researchers are Rice and Drs. Nicholas Vedder, John Harlan and Robert Winn. They, along with a handful of other scientists around the country, are reporting promising results. Someday, various forms of anti-adhesive therapy could help save thousands of patients—human and animal—who are struggling to recover from such common medical conditions as cardiac arrest, stroke, burns, massive infections, arthritis and even frostbite. This therapy could also soften the blow of major surgery, including organ transplants and limb reattachments.
Anti-adhesive therapy counteracts inflammation, the body’s natural response to injury. When normal blood flow is interrupted, either to a limb or throughout the entire body, the immune system dispatches a special type of white blood cell to carry off dead tissue and help fight infection.
These cells, called polymorphonuclear neutrophils (PMNs), try to clean up the wounds. The body sends them where they are needed, just as the state patrol sends a patrol car to the scene of an accident.
This normal response is essential to recovering from injuries. But when injuries are especially severe or generalized—as in severe blood loss (hemorrhagic shock), cardiac arrest and other conditions—the special white blood cells can run amok. “An overexuberant inflammatory response, while intended to be efficient for cleaning up dead tissue and fighting infection at specific sites, gets out of hand and, in fact, does harm,” says Vedder, an assistant professor of surgery who specializes in plastic, reconstructive and hand surgery at Harborview.
Dr, John Harlan
Following restoration of normal blood flow after shock, the white blood cells can proliferate throughout the body’s vast vascular network as well as at the site of injury. They cling to the walls of tiny blood vessels and release toxic substances that damage blood vessels and impair organ function. It would be like sending out thousands of patrol cars in all directions rather than just to the scene of an accident. Instead of helping the victims and getting traffic moving, the cars add to the traffic congestion and cause a transportation breakdown.
Enter “the juice”—MAb 60.3—which thwarts this natural process. Normally, the white blood cells lock, Velcro-like, into interlocking receptor sites along the vascular wall. But MAb 60.3 caps or coats the errant white blood cells in such a way that they can’t possibly adhere while the drug is active in the body.
“MAb” is scientific shorthand for “monoclonal antibody,” a term that applies to a broad class of genetically engineered molecules. In the laboratory, such substances can be designed to target a theoretically infinite array of undesirable cancer or other types of cells.
As Rice and his UW colleagues reported in a recent issue of Surgery, this particular monoclonal antibody, MAb 60.3, prevents dangerous inflammation—and potentially fatal organ damage—by quickly attaching to the rogue white blood cells and keeping them from clinging to walls of the body’s network of veins.
In the Surgery study, MAb 60.3 injections were given to five anesthetized rhesus monkeys who were in shock from temporary blood withdrawal. A control group of five other monkeys received the same treatment, except instead of MAb 60.3 they received an equal volume of saline solution. In keeping with the usual practice in scientific studies, the scientists did not know at the time which animals received the substance and which did not.
* * *
All of the monkeys in the Surgery study—members of a species numerous in the wild—were bred for research and housed at the UW’s Regional Primate Research Center, one of seven such facilities established by the federal government at leading research institutions. The animals’ medical treatment following induced shock was similar to the treatment humans receive, with the exception of MAb 60.3.
All five monkeys given MAb 60.3 survived with no evidence either of stress gastritis—a common, usually treatable complication of hemorrhagic shock—or other organ damage. But all five control animals had gastritis as well as other complications; two in this group died from multiple organ failure syndrome within 72 hours. One of the therapy’s first applications, the UW researchers hope, will be using MAb 60.3 to treat patients whose traumatic injuries involve severe blood loss and a rapid decline in blood pressure, leading to hemorrhagic shock. If all goes well, such treatment could be widely available within just a few years.
MAb 60.3 was developed in 1983 by Dr. Patrick Beatty, UW associate professor of medicine and an associate member of the Fred Hutchinson Cancer Research Center, with colleagues from the UW. Originally, it was intended for quite a different purpose: as a basic research tool. Its first clinical application—which was unsuccessful—was an attempt to help patients undergoing bone-marrow transplantation.
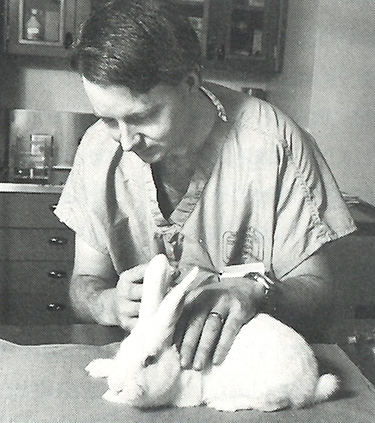
Dr. Nicholas Vedder
In John Harlan’s view, the seemingly wondrous qualities of “the juice” might have gone undetected without the collaboration that routinely occurs among physician-scientists at various Seattle-based institutions, including (in this case) the UW, the Hutchinson Center and the Puget Sound Blood Center.
In 1982, a group of UW researchers that included Pediatrics Professor Hans Ochs published an important study. They described an inherited condition in which certain white blood cells failed to properly adhere to vascular walls. “They were one of the first groups to describe a patient with this condition,” says Harlan, a professor of medicine and head of hematology at the UW.
In 1985 researchers in Harlan’s laboratory first showed that MAb 60.3 inhibited PMN adherence to blood vessel walls. Members of this group went on to publish another study in the British journal, Lancet, showing that “the juice” actually mimicked the inherited defect described in the Ochs’ study. In addition to Harlan, that group included Beatty and UW Medicine Professor Thomas Price, director of clinical services at the Puget Sound Blood Center.
Last year, Vedder and other members of the group—now known throughout the world among specialists as “the Seattle Group”—published the monkey study and went on to show that 60.3 greatly enhances recovery after surgical reattachment of rabbit ears. This could lead a better success rate in reattaching severed limbs in humans.
“Anti-adhesion therapy has become a very exciting, potentially new approach to a wide variety of immune and inflammatory diseases, prompting a biotechnology frenzy,” says Harlan. “The message is that the willingness to share data and collaborate allowed investigators here, in a variety of disciplines, to develop a promising approach to therapy for a potentially very diverse group of disorders. All of us in the Seattle Group are very proud, I think, to be playing a major role as one of the leading investigative groups in this field.”
At present, it’s still a painstaking process to manufacture MAb 60.3. Starting with a cloned cell line developed by Beatty, specially bred mice receive cell injections that form tumors. These tumors, in turn, are capable of rapidly producing the antibody which, when syphoned from the tumor and purified, becomes the clear liquid called MAb 60.3.
“It’s an extremely potent drug—as far as we know, the most potent anti-inflammatory therapy developed to date,” says Vedder. “When it’s injected intravenously into rabbits or monkeys, only a couple of CCs bind to all the white blood cells in the animals’ bodies instantaneously.”
This powerful effect has both its pluses and minuses, Vedder quickly mentions, and points the way for additional research before the drug can be tested in humans.
“In a sense, we’re in the process of trying to ‘finetune’ evolution,” he comments. “It’s important to keep in mind that when you’re tinkering with a basic body response like this, there always will be some risk involved, because that response has evolved over the millennia and it’s there for a reason.”
One of the biggest hurdles, Vedder notes, is that many trauma patients need to have the infection-fighting capabilities of PMNs. “These patients are at increased risk of infection, but with 60.3 we’re going to inhibit the body’s normal immune response. That’s clearly an issue we’re in the process of addressing, along with determining such things as the best time to administer the drug and optimal dosages.”
On the other hand, those properties that inhibit the body’s inflammatory response might be used to treat septic shock from massive infections. “It might seem rather contradictory that one of the major risks of this antibody is infection, when we’re hoping to use it to treat overwhelming sepsis (infection) itself,” Vedder notes. But with an overwhelming infection, inflammation can often kill the patient, he adds, and the juice’s primary effect is to ameliorate that response.
If they obtain approval from the U.S. Food and Drug Administration, Vedder and the others hope to begin human clinical trials of the drug within the next year or so. It could become widely available for trauma patients within three to five years, they believe.
As the research goes forward, the scientists keep their eye on an inescapable fact: Trauma affects younger generations disproportionately. It is the leading cause of death for Americans under age 30. “The juice” just might send this fact to the archives.