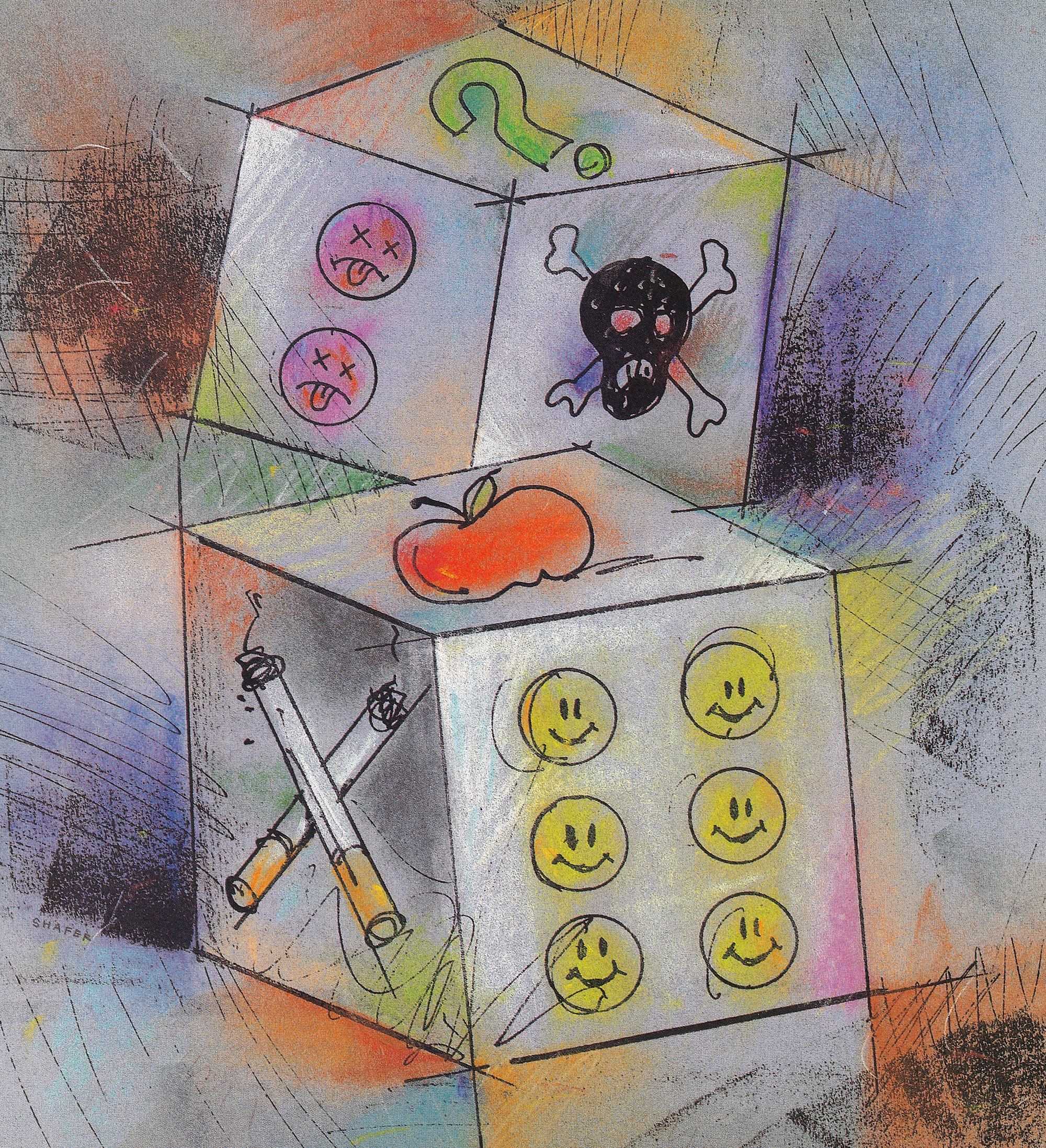
Risky business Risky business Risky business
Peanut butter or bacon is more dangerous than a glass of juice from Alar-treated apples, say UW experts, who want to clear the air about environmental risks.
By Cheryl Dawes | Illustration by Ken Shafer | March 1993 issue
Some people are willing to leap from a tower 100 feet above the ground with only a bungee cord between them and certain death. Yet this same bungee jumper who eagerly takes that leap of faith may not be willing to live near a closed mill that has been declared a Superfund site.
Or consider the smoker who continues to puff while worrying about pesticide residue on her apples. Public health experts generally consider smoking the number one health hazard facing Americans.
Some risks are accepted and even sought out, yet others spark fear and anger. Why such a difference in response to risk?
If personal benefits seem to outweigh the dangers involved, a person is likely to disregard risks, points out Dr. Dave Eaton, a toxicologist and UW professor of environmental health and environmental studies. We are also more likely to accept risks we choose—such as bungee-jumping—rather than those imposed on us.
Without a background in toxicology it’s hard to evaluate the danger of environmental health risks emblazoned in startling headlines. It’s no easy task even for toxicologists.
For example, in 1989, the highly publicized controversy over Alar-treated apples and cancer sparked a chain reaction of fear and confusion. Apple sales plunged, resulting in a $130-million loss for Washington’s apple industry.
But the risks trumpeted by “60 Minutes” and others were not nearly as significant as media coverage seemed to indicate. Juice made from Alar-treated apples is about as dangerous as chlorinated tap water, Eaton estimates. He points out that making an estimate of the actual level of risk (probability of getting cancer in a lifetime) posed by eating Alar-treated apples or drinking juice from those apples is difficult and depends upon many uncertain assumptions.
So what’s a consumer to think?
Eaton, who has chaired the science advisory board for the state Department of Ecology, has seen first-hand how scare tactics and hyperbole can sway voters. “The environmental movement has made incredible changes in the laws of this country,” says Eaton. “The vast amount of them are good. But we shoot ourselves in the foot by setting standards that are too stringent and expensive to meet.”
He wonders whether it makes good sense to devote large amounts of resources and time to cleaning up contaminated sites to “pristine” levels. Somewhat less stringent cleanup levels may be reached much sooner—often at only a fraction of the cost—without significantly compromising public health or environmental quality. He also questions the wisdom of writing regulations that reduce incentives for polluters to conduct their own cleanups, thus escalating litigation costs and cleanup time.
Confusion often arises as scientists mouth terms that mean nothing to the public. Dr. Gilbert Omenn, dean of the UW School of Public Health and Community Medicine, recalls a case in 1985 when the Environmental Protection Agency (EPA) presented proposed regulations for control of arsenic emissions from a Tacoma smelter. In a series of public workshops, “The scientists spoke in terms of a risk assessment of 2.73 times 10 to the minus something or other,” says Omenn. What the public wanted to know had nothing to do with numbers. They wondered if it was okay for the kids to play outside or if it was safe to eat vegetables from their gardens.

A grocer at Larry’s Market in Seattle adjusts Alar-free apples in the produce bins. UW scientists say juice made from Alar-treated apples is about as dangerous as chlorinated tap water.
All too often, the public doesn’t get an explanation of the inner workings of risk assessment.
Federal agencies gave birth to the current risk assessment framework during the Carter administration in the late 1970s. Omenn, who served as a health and science policy advisor in that administration, was a midwife in that process.
The basic framework consists of three major steps: identify a hazard, characterize its risk and take actions to reduce that risk. First, scientists determine if a certain chemical in sufficient dosage, under sufficient exposure, produces adverse effects. According to the Toxic Substances Control Act, all new chemicals must be tested for toxicity. However, in order to avoid exposing humans, scientists expose animals or bacteria to the chemical compound in question and then infer the results for humans, Omenn notes.
For chemicals already in use, epidemiological studies may be possible. These studies analyze the chemical’s effects on humans who have been exposed, often in the course of work. Such studies have their limits, though. Studies on low levels of exposure often require an infeasible number of subjects in order to be statistically valid. In addition, cancer can be caused by a combination of factors, as well as by the chemical in question. These other risks must be factored into any study.
After risk assessors identify a hazard, the second step is to characterize the risk. What is the smallest dose of a chemical that will cause an adverse effect in humans? In order to make the most efficient use of expensive and time-consuming animal studies, toxicologists test very high doses of substances on small numbers of animals, under controlled conditions. They then attempt to extrapolate the results to the very low doses that humans may receive.
“When it comes to risk projection and statistical associations, it's very easy to get bamboozled.”
Gilbert Omenn, dean of the UW School of Public Health and Community Medicine
Translating from animals to humans has its pitfalls. The amounts that cause cancer in animals may be a thousand times greater than the amounts ingested or inhaled by humans. Also, the picture becomes fuzzier when, as in the case of a chemical in unleaded gasoline, the substance produces tumors in male rats only—not in mice, not in female rats and not in humans.
In addition to looking at dosages, scientists try to measure or estimate exposure levels over an average lifetime. Pinpointing appropriate levels can be tricky because, unlike the animals in controlled studies, not all humans eat the same food, breathe the same air or work in the same conditions.
The third step, managing the risk, is a balancing act that, Omenn says, is better separated from the more scientific previous steps. Risk managers weigh the costs and benefits—social, economic and political—associated with the use or cleanup of substances that pose some degree of danger.
The uncertainties and scientific limitations prompt risk assessors to build in extra safety factors and take a conservative approach, says Omenn. Nevertheless, he notes, despite shortcomings, risk assessments provide a useful basis for policy makers as they make the calls on how to protect human health and the environment.
The risk assessment process itself is under constant scrutiny as scientists search for ways to improve measurements and estimates. For instance, Omenn and other researchers in the UW School of Public Health are working on part of the process. They are looking at variability among individual humans and asking how each person’s biological heritage affects his or her susceptibility to environmental exposures.
Omenn’s experience in the “other” Washington taught him an important lesson. There must be better training for those who do risk assessments—and those who use them. To help, he and Dr. Elaine Faustman, a UW environmental health professor, developed a graduate-level course that reaches across disciplines. It attracts students in public health, engineering, public affairs and environmental studies.
Many of the students already have real-world experience and have come to graduate school after working in regulatory agencies or consulting firms. “Although they won’t be doing every aspect of risk assessment themselves, we try to help them understand how to be critical, ask good questions and be able to find mistakes. When it comes to risk projection and statistical associations, it’s very easy to get bamboozled,” says Omenn.
The course also places a strong emphasis on risk communication as a two-way process. “Scientists and policy makers have to listen as well as talk,” says Omenn.
Younger students also should learn the basic principles of risk assessment, says Eaton. Last year he was named the first Rohm and Haas Distinguished Professor in the Public Health Sciences, in part because of his proposal to help teach risk fundamentals in middle school and high school. He hopes that young people learn to recognize that it’s essential to get at the gist of the scientific problem and its possible remedies—no matter who is the “bad guy.”
Eaton, Omenn and others admit that risk assessment can be a maze of statistics. That’s why, they say, it’s important to look beyond the headlines when making decisions about the risks that affect all of our lives.
Putting a number on risks
Putting an absolute number on the dangers of a particular substance is, well, a risky business. Numbers can’t express the uncertainties that come with extrapolating animal studies to humans. But, by looking at the hazard posed by environmental substances in terms of relative risk of causing cancer, we can get an idea of the risks that pose the greatest danger.
Seymour Garte of the New York University Medical Center has invented an easy way to express environmental risks. He suggests a scale of relative risk similar to the Richter scale for earthquake intensity. Because risk is related to amount of exposure, Garte used estimates of average daily intake for several well-publicized environmental hazards to construct his scale.
Like the Richter scale, Garte’s scale is logarithmic. A substance with a relative carcinogen risk value of “2” poses a risk 10 times greater than a substance with a value of “1.” Values greater than 5 indicate a serious risk of cancer, values of 3 to 4 represent moderate cancer risk and those less than 2 can be considered minor when compared with background risks.
- 6.1: Ethylene dibromide or EDB (pesticide used on grains) occupational exposure
- 5.8: Cigarette smoking (2 packs per day)
- 5.0: Asbestos, occupational exposure Formaldehyde in mobile homes
- 2.8: Saccharin in one soft drink
- 2.5: Aflatoxin in one peanut butter sandwich
- 2.0: Nitrosamines in one serving of bacon
- 1.2: Alar in one glass of apple juice
- 0.7: Ethylene dibromide (EDB) exposure from dietary intake of residue