Hope in fight against Alzheimer's Hope in fight against Alzheimer's UW research offers hope in the fight against Alzheimer’s
Almost half of all Americans over 85 have Alzheimer's, but hope is on the horizon as UW research begins to break its secrets.
By Jon Marmor | March 1995 issue
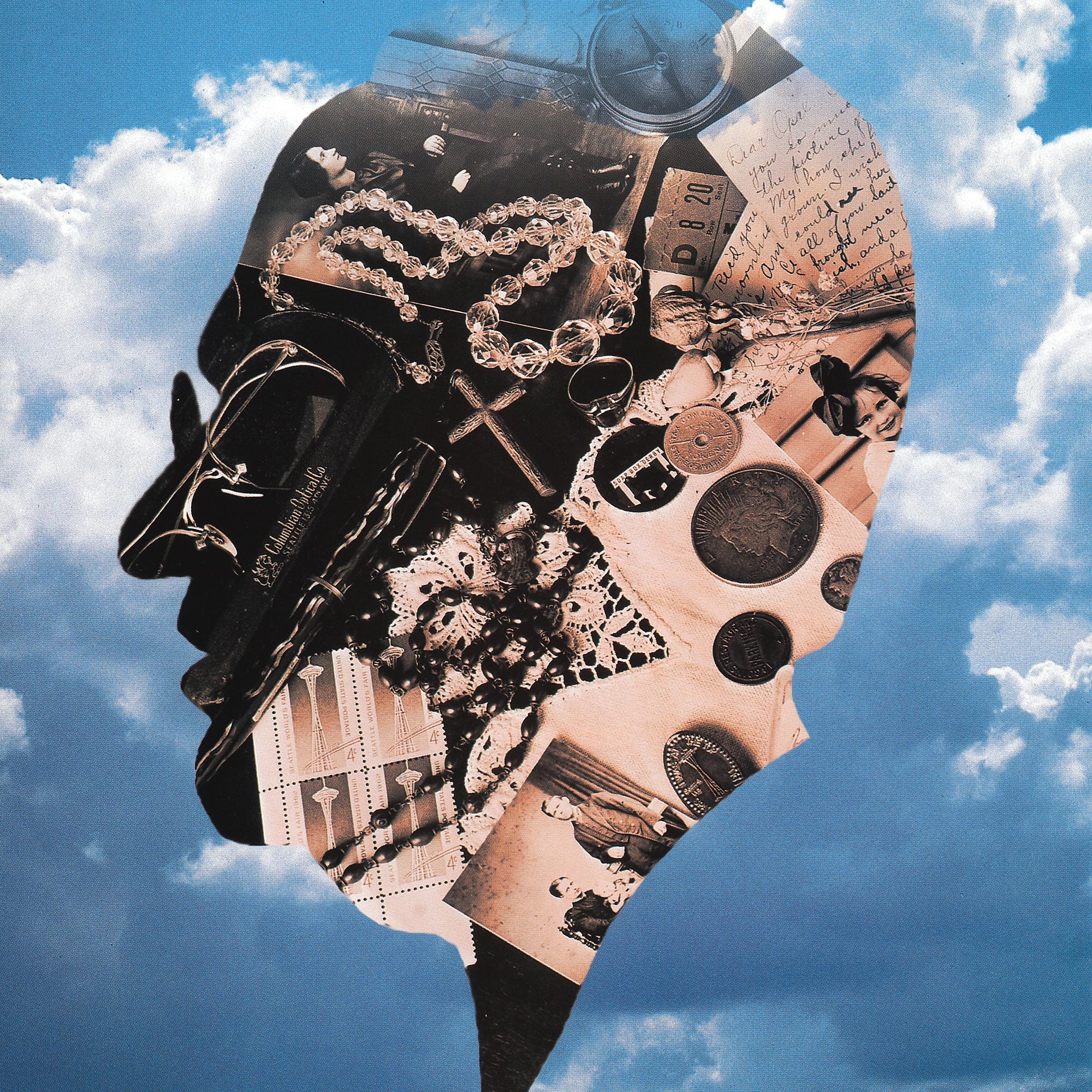
July 4: It's fireworks, parades, picnics, softball, three-legged races, a day with the family on a blanket in a park. Hot dogs on the grill. Playing frisbee. The good things in life. For Sandra Lewis, however, one recent Independence Day meant the beginning of dependence.
Until then, she had paid little attention to the memory problems her father was having. On a bright, recent July 4, her parents were off to attend a wedding at the Seattle Yacht Club. What could be better than getting together with friends to celebrate one of life’s joyous occasions, at the dazzling backdrop of Portage Bay?
Her father, a Seattle native, drove. He got lost.
“That’s when I knew something was very wrong,” says Lewis. Her wall of denial came crashing down like a window shattered in an earthquake. “I didn’t want to face the fact that my father’s problems could be serious.”
Within weeks the word came from the doctors: Her father was one of about 4 million Americans suffering from Alzheimer’s disease — an incurable, progressive, degenerative disorder that attacks the brain and results in impaired memory, thinking and behavior.
“It is very clear there are genetics involved. But we don't know them all, or why they function as they do. But we are on to something.”
Tom Bird
That came on top of the fact that her mother was suffering from a similar form of dementia. Sandra’s parents now reside in a Seattle-area nursing home, and she visits them twice a week.
It’s a heartbreaking situation that Tom Bird knows all too well. As a professor of neurology at the University of Washington, he runs a clinic for older people with neurological problems. He is intimately familiar with the pain, the frustration, the devastation of Alzheimer’s.
But there is a glimmer of hope. Research conducted at the University of Washington — as well as worldwide — has yielded new levels of understanding of this complex, difficult disease.
When he isn’t treating patients, Bird is among a small research army at the UW working to uncover the causes of — and develop treatments for — Alzheimer’s. Bird’s unit is delving into the root causes — in the genes.
“It is very clear there are genetics involved,” Bird explains. “But we don’t know them all, or why they function as they do. But we are on to something.”
The UW’s genetic research is focused on a strain of the disease passed down from generation to generation: specifically, families with three family members with the disease in two generations. By studying those families, where the link clearly is genetic, researchers believe they can home in on some vital clues.

Tom Bird
“Alzheimer’s is a pretty common disease,” says Bird, noting that 10 percent of all people over 65 and 47 percent of those over 85 have the disease. “But that wasn’t what we were taught in medical school.
“Back then, I learned it was not a common occurrence, and that only people younger than 60 came down with what was known as senile dementia.” In other words, Alzheimer’s was probably always around, but not considered as a disease. There is an ever-growing number of Alzheimer’s cases today, largely because people are living a lot longer.”
Since 1907, scientists have known about the physical changes that occur in the brains of Alzheimer’s patients. That’s when a German psychiatrist named Dr. Alois Alzheimer did an autopsy on a woman who died following a mysterious mental disorder. He found abnormal deposits of a sticky plaque along with odd masses of tangled nerve fibers.
Later on, pathologists studying the brains of people who died of “senile dementia” noticed the same thing. Scientists realized that these findings were the results of the same disease — Alzheimer’s.
Today, there still is no cure and no real way to treat the condition. But over the past 10 years, after the National Institutes of Health poured money into Alzheimer’s research, progress has been dramatic, researchers say.
Three years ago, UW scientists made a landmark discovery about the genetics of early-onset Alzheimer’s in families. They located a mutation in a region on human chromosome 14 that was linked to this variety of the disease. Researchers found that 90 to 95 percent of the cases of early-onset (some as young as 40 years old) were caused by these abnormalities.
“There are so many clues emerging now,” says Pathology Professor George Martin, director of the UW Alzheimer’s Research Center. “And this is not an easy disease to understand.”
Unlocking the mystery of Alzheimer’s is difficult for a variety of reasons. First, its symptoms can be caused by a litany of conditions common to older people — depression, stress, side effects from medication, strokes, Parkinson’s disease, to name a few. It only can be diagnosed with 100 percent accuracy through an autopsy. Many people with nerve fiber tangles and plaques in their brains may die before they come down with the disease. And there are multiple genes known to be involved in different forms of Alzheimer’s, according to Dr. Ellen Wijsman, the UW research’s team’s genetic statistician.
To make their mystery easier to solve, UW geneticists are concentrating on Alzheimer’s in families. More than 600 families — like the Lewises — have volunteered to let the UW study them. Of that number, 87 families met the criteria the team needed — at least three Alzheimer’s-affected individuals in two generations.
“People call and want to get involved because they want to help someone else avoid what they are going through,” says Ellen Nemens, a nurse who interviews families for the study. “There isn’t anything we can do for them, but they are making an incredibly big contribution.”
After family histories are taken, medical records and blood samples are collected. The UW provides no medical care, leaving that to the families’ personal physicians.
“Now that we have identified regions, we have to try to pinpoint the gene. It will happen. It is just a matter of time.”
Jerry Schellenberg
Then Jerry Schellenberg, a UW research associate professor with a background in molecular biochemistry, and his lab begin the tedious detective work of analyzing DNA material from families. “It takes a long time to go through all the information we have,” Schellenberg says. “Now that we have identified regions, we have to try to pinpoint the gene. It will happen. It is just a matter of time.” But it could be a long time since the area of the chromosome 14 with the mutation could contain more than a million genes. The task is to find the needle in that genetic haystack.
“We are getting closer than ever,” Schellenberg says. While the exact problem in the gene isn’t known, Schellenberg’s hunch is that it has something to do with the formation of beta amyloid, the protein plaque found in the brains of Alzheimer’s patients during autopsies.
“We are trying to find out what destroys existing brain structures,” he adds. And that means tedious, painstaking work with DNA in test tubes.
If and when the gene is found, he says that biochemical research can develop drugs that could affect the gene in question, perhaps a drug that could limit the debilitating effects of the disease. Or better yet, find a drug that could prevent the disease.
The UW lab is also looking at two other chromosomes — 19 and 21 — where other defects have been associated with Alzheimer’s. But there have been other, surprising clues that don’t appear to be related to chromosomes 19 or 21. UW researchers are studying a number of families with Alzheimer’s. About 500 German immigrants settled two centuries ago into the villages of Frank and Walter in Russia’s Volga Valley. They later came to the U.S. and settled in the Midwest. About 200 descendants of these U.S. families are being studied.
Some of these “Volga Germans” have Alzheimer’s, but it isn’t due to problems with chromosomes or proteins associated with many Alzheimer’s patients, according to the UW’s Bird. “It has to be something else,” he said. “We don’t know what it is. It is genetic, but it isn’t connected to the other cases we have. That means there is some other genetic link we have to find.”
The first big breakthrough in genetic analysis of Alzheimer’s came in 1991 when English scientists found a mutation in an amyloid gene that affected a protein in the brain. If that gene was inherited, chances were high that a person would come down with Alzheimer’s by age 60.
Lately, attention is being focused on a protein called apo E, which transports cholesterol in the blood. People with one type of this protein, called apo E4, are more likely to have Alzheimer’s in old age than others, according to Duke University scientists. Their findings showed that Alzheimer’s patients with two copies of the apo E4 protein (one from each parent) were likely to come down with Alzheimer’s by age 70.
But no one knows what apo E4 does, says Alzheimer’s Research Center Director Martin. Plus, there are many people with Alzheimer’s who don’t have this apo E4 protein. So finding the protein may not have much diagnostic value.
“This is what makes this so complicated,” says Sandra Lewis, who in addition to having both parents suffering from dementia, is executive director of the local Alzheimer’s Association chapter. “There also could be environmental factors involved. But no one knows.”
Environmental factors certainly have stirred a lot of media attention and interest by the general public. For a while, some people were convinced that exposure to aluminum caused Alzheimer’s, based on the findings of aluminum deposits in brains of some Alzheimer’s victims. But it isn’t clear if this happens consistently or if the mineral deposit was a cause — or an effect — of the disease. Another study, at Massachusetts General Hospital in Boston, suggested that zinc might somehow initiate the clumping of certain proteins in the brain, which is associated with the death of neurons. But that study was a test-tube study, not an experiment with humans. “What happens in a test tube may or may not happen in a living brain,” says Dr. Zaven Krachaturian of the National Institute of Aging. While zinc has been found to cause clumping of proteins in-vitro, “it is premature to say anything about zinc and Alzheimer’s,” he explains.
Using patients in the Group Health Alzheimer’s Disease Patient Registry in Seattle — a joint project of the UW and Group Health since 1987 — UW researchers are looking to see if exposures or lifestyles may be at the heart of the disease. Focusing on such things as smoking, chronic depression, education, exposure to solvents, alcohol, and head trauma, some small statistical links have been detected, but not enough to clearly state one of these causes the disease.
Studies continue into drugs that could diagnose the disease and treat it. Researchers in Boston have found that some people diagnosed with probable Alzheimer’s exhibited a sensitivity in their pupil dilation when a drop of tropicamide was put in their eyes. That study continues. Closer to home, Psychiatry Professor Murray Raskind, associate director of the UW Alzheimer’s Research Center, has tested a number of treatments for Alzheimer’s patients. Tactrine, a drug partly developed at the UW, is the only drug approved by the Federal Drug Administration. It increases memory and alertness in about one-third of the patients in the early stages of the disease. In addition, the UW center is testing another drug, Sabeluzole, which has prevented brain-cell death in laboratory rats.
As the hunt in the labs continue, people like Sandra Lewis are overwhelmed trying to deal with caring for people who forget where their car keys are, don’t remember to eat or go to the bathroom, or exhibit other strange behavior, such as asking the same question repeatedly.
“Remember what it was like caring for a baby?” asks Lewis. “Well, think of someone that way who is six feet tall and weighs 150 pounds. It is overwhelming. I never used to miss work, but I had to start missing work to care for my father before he was put in a nursing home.”
With the announcement by former President Ronald Reagan that he has been diagnosed with Alzheimer’s, “people have been coming out of the closet like crazy,” Lewis says. “People are desperate for knowledge. And the effect on families is just awful. In my own family, there has been a huge battle with other siblings over the care of our parents. And the costs for their care is incredibly expensive, maybe as much as $4,000 a month for a nursing home.”
Sandra Lewis collects herself for a moment. “There isn’t much that can be done now for people like my father. But if there is any way we can contribute to finding out what causes this disease, and preventing it in the future, we will do anything we can.”
Alzheimer’s warning signs: It’s more than lost car keys
There is more to Alzheimer’s disease than just a bad memory. Since many conditions can cause Alzheimer’s-like symptoms — such as adverse drug reactions, depression or stroke — an accurate diagnosis by a neurologist or a physician experienced at dealing with patients with memory problems is essential.
“Some people worry that because they forgot where they put their car keys that they have Alzheimer’s,” said Dr. Tom Bird, a UW professor of neurology conducting research into the genetic causes of the disease. “The majority of the time, that isn’t the case.”
The Alzheimer’s Association has developed a list of 10 warning signs that some form of dementing illness may be present. They are:
- Recent memory loss that affects job skills
- Difficulty performing familiar tasks
- Problems with language
- Disorientation of time and place
- Poor or decreased judgment
- Problems with abstract thinking
- Misplacing things
- Changes in mood behavior
- Changes in personality
- Loss of initiative