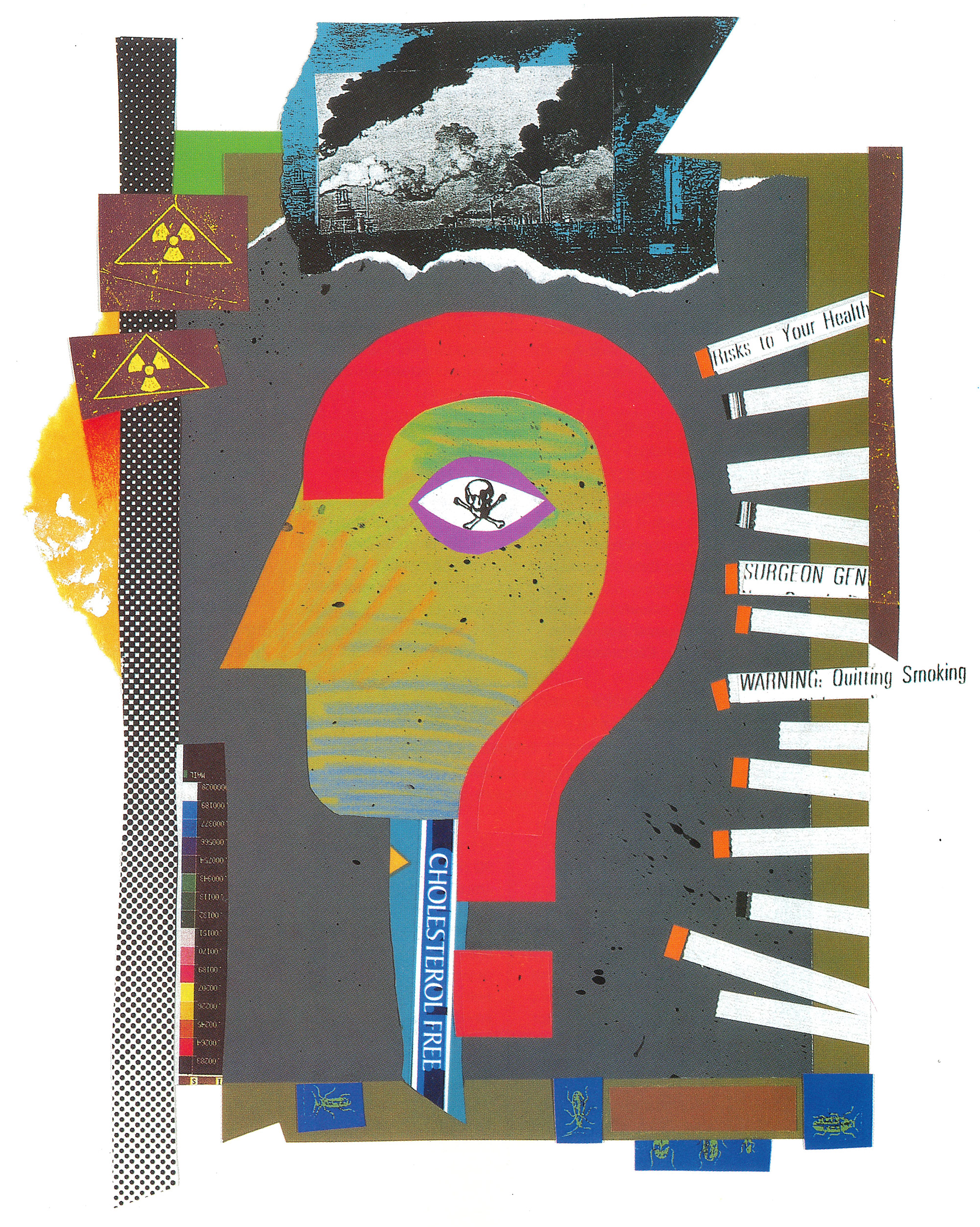
Why me, doc? Why me, doc? Why me, doc?
The University of Washington is home to the nation’s first concentrated research effort in the budding field of ecogenetics.
By Sabrina Porter Lindquist | Illustration by Ken Shafer | June 1990 issue
Physicians dread hearing the following impossible—but common—questions from patients:
- “My neighbor smokes three packs of cigarettes a day and he’s never been sick a day in his life. I cut back years ago and now you tell me I have lung cancer?”
- “I didn’t know I was pregnant when I got drunk at my friends’ weddings. Is my baby going to be all right?”
- “Each time I spray my fruit trees with insecticide I start coughing and feel dizzy. What’s wrong?”
UW Dean Gil Omenn, himself an M.D. and a former health-policy adviser to President Jimmy Carter, says he has been asked the same types of questions many times: “Why me, Doc?”
“As more medical conditions are associated with environmental exposures, people want to know ‘Why me?’,” says Omenn, dean of the School of Public Health and Community Medicine. “They say, ‘I’m no more exposed than anybody else’ or ‘I’m no less careful than anybody else on the job.’ We owe patients a good try at an answer, especially if there is something they can personally do, short of changing the whole world, to protect themselves.”
Dr. Gil Omenn
Thanks to Omenn and Dr. Arno Motulsky, a leading medical geneticist, the University of Washington is home to the nation’s first concentrated research effort in the new field of “ecogenetics.” Ecogenetics is the study of connections between environmental elements—such as cigarette smoke, alcohol, food, pesticides, the quality of the air itself—and the unique features of each person’s inherited biological makeup.
Each of these factors is complex in itself. Together, they present a formidable research challenge. For example, the first evidence linking cigarettes and lung cancer surfaced 40 years ago, but scientists still don’t know exactly which of the 4,000 chemicals in cigarette smoke are responsible. Neither do they understand why smoking causes nine out of 10 cases of lung cancer, but only one in 10 heavy smokers gets it.
Despite the complexity, this research by 20 or so scientists from the schools of Medicine and of Public Health and Community Medicine could change the way we live. In the future, physicians might be able to test patients for dangerous vulnerabilities to various common chemicals. On a larger scale, the work may redefine environmental law and public health policy. But it also could open a Pandora’s box of abuse by employers, insurance companies and irresponsible individuals.
Research in ecogenetics demands more knowledge and skills than any single scientific discipline imparts. This is where the UW program, the first of its kind in the nation, fills the gap. With a $650,000 grant from the Charles A. Dana Foundation awarded in 1985, the UW brought together toxicologists, geneticists and epidemiologists.
“It’s a concept whose time has come,” says Dr. Curt Omiecinski, a pharmacologist and environmental scientist who studies how human enzymes break down environmental toxins.
“Researchers talk about an integrative approach but don’t really do it. We tend to work on our own little problems in our own little worlds.”
The UW group is studying differing risk thresholds in three major areas: lung cancer from chemicals in cigarette smoke and other exhausts, nervous system damage from pesticides, and birth defects from alcohol and certain medications.

Dr. Arno Motulsky
This hybrid approach differs from the typically more narrow focus of medical research. Motulsky, a UW professor of medicine and genetics who directs the project, explains the difference. “An epidemiologist, for example, would ask what in the environment makes you sick,” he says. “The ecogenetic question is why only some people who are subjected to an environmental agent get sick. It’s not so easy to have clean proof.”
Clean proof is rare in research, but the UW project has produced encouraging results in several areas. One factor in lung cancer may be an enzyme—called glutathione transferase—which helps the body dispose of tobacco smoke byproducts. Approximately half the population normally doesn’t have one form of the enzyme. UW researchers suspect people who lack it may have a higher chance of contracting lung cancer from smoking.
UW researchers also have found that about half the Caucasian population bas a less active form of paraoxonase, an enzyme that breaks down certain common pesticides. These people don’t readily rid themselves of pesticide byproducts, and so may be at higher risk of a toxic reaction.
In each case people are vulnerable due to differences in a single gene. Such inherited differences have been overlooked thus far in environmental medicine, says Motulsky, who founded the project with Omenn. Motulsky’s longstanding interest in genetic differences in drug responses and in risks for common adult diseases set the stage for ecogenetics.
“In the last 20 years, we've come to realize that our internal makeup is just as unique as our external makeup.”
Dr. Arno Motulsky
“We all accept that we look different,” he says, “and that we inherit our appearance from our parents. In the last 20 years, we’ve come to realize that our internal makeup is just as unique as our external makeup. … Environmental agents don’t act in a vacuum. They act against a genetically determined, variable background.”
Cigarette smoke certainly qualifies as a high-risk environmental agent. Dr. David Eaton, UW associate professor of environmental health, is trying to find out why 90 percent of heavy smokers manage to escape lung cancer.
The body rids itself of tobacco toxins by disarming them with enzymes. But for some smokers, certain enzymes fail to neutralize the presumed carcinogens. During processing, other enzymes may turn harmless chemicals in smoke into toxic compounds. Eaton is looking at how much of each type of poison finds its way to DNA, the body’s storehouse of genetic information, where long-term damage occurs.
This critical dose of carcinogen usually is a very small fraction. One person may detoxify 99 percent and another person may detoxify 98 percent of the same dose. The leftover doesn’t seem like much, Eaton notes, nor does the 1 percent difference. But the latter person actually has double the amount of carcinogen—2 percent vs. 1 percent—in his or her system, he points out, and small differences in enzyme efficiency can mean large amounts of DNA damage.
Alcohol is another environmental risk. Nearly 20 years ago, three UW pediatricians were first to identify fetal alcohol syndrome, a group of birth defects characteristic of alcohol damage. Now scientists, including second-year medical student Leticea Stevenson, are looking for a link between such defects and genetic differences in the way the body processes alcohol. Stevenson, who is of Native American heritage, was interested in the problem because of the high incidence of alcohol-related fetal damage among ethnic populations. She heard about the research project and sought out Dr. Elaine Faustman, the developmental toxicologist who heads the project.
Researchers theorize that the mother’s genes may make her baby more susceptible to fetal alcohol syndrome. As with cigarette smoke, certain enzymes attack alcohol in the body, alter it chemically, and control the rate of eliminating byproducts. One byproduct is acetaldehyde, which Faustman suspects may cause fetal damage. She theorizes that mothers with alcohol-affected children—and the children themselves—have more acetaldehyde in their systems for a longer time than would a “normal” person after the same drink.
To test her theory, Faustman takes blood samples from alcoholic women who drank during pregnancy and from their children. She analyzes DNA in the blood cells for clues to each mother’s alcohol-processing capabilities and for a link to the alcohol-related damage their children suffer. Attempts to track down the alcoholic mothers have led to taverns, prisons and, in more cases than would be expected among women in general, the morgue. “It’s very, very sad,” she says. “Some of the mothers feel guilty and devastated. Some also have a very strong commitment to try to help the research and want to do anything they can.”
Faustman’s work may lead eventually to a test that will tell women how sensitive they are to alcohol, and thus how vulnerable their unborn children are to related birth defects. Such a test could be a useful preventive measure, but Faustman also acknowledges that women shown to be less vulnerable might view the results as a license to drink.
Confounding public-policy questions are common to ecogenetic research, though there are many potential advantages. With a blood sample or other simple test, physicians eventually may be able to profile their patients’ personal thresholds to chemical threats in their food, homes, neighborhoods, workplaces or lifestyles. Those tested could use the results to make better choices about their health. Employers could create safer, healthier working conditions. Regulatory agencies could set health and safety standards with more assurance that they protect everyone.
On the other hand, some people may ignore specific health warnings—just as many smokers now ignore the surgeon general’s warning on cigarette packs. Even worse, some people might believe that low susceptibility means they are invulnerable to a disease. Employers could use risk thresholds to discriminate in hiring. Insurers could use the same information to deny coverage.
Omenn, an international authority on health-risk assessment, has considered these scenarios. He cites the limited success of public-health messages against drinking and smoking as evidence of the need for ecogenetics research.
A warning is much more powerful in an individual context, Omenn says, such as when a person seeks genetic counseling because a disease runs in the family. People tend to be motivated to change by specific information, he says.
In the workplace, Omenn expects that the results of ecogenetics research are more likely to be used for constructive, rather than harmful, purposes. Laws protecting privacy and prohibiting job discrimination are in place, he notes, and covert testing would take “a remarkably determined effort.”
Knowledge of individual thresholds to certain job-related hazards could help steer job applicants away from harmful work, Omenn says. If a small number of workers were shown to be vulnerable to a job-related chemical exposure, they would serve as “sentinel cases” and signal a need to protect workers with higher thresholds from more intense or longer exposures.
The quandary over public policy factors, however, is no excuse for physicians, Omenn says. “It is not ethical for us as physicians and biomedical scientists to tell patients we don’t care to answer their question when they ask ‘Why me?'”