UW Medicine among first to deploy drug that slows Alzheimer’s
Doctors at UW Medicine are among the first to treat patients with a new drug that slows the progression of Alzheimer’s. They describe it as a first step toward revolutionizing the treatment of the disease.
“In many ways, Alzheimer’s disease is the biomedical challenge of our time,” says Dr. Thomas Grabowski, ’88, director of the UW’s Alzheimer’s Disease Research Center and Memory & Brain Wellness Center. In the U.S., about 6.5 million people—and one in nine over 65—are living with Alzheimer’s dementia. That number is expected to grow to 14 million by 2060. It is one of the leading causes of death.
But while scientists have made significant progress developing treatments for cancer, heart disease and diabetes, they are decades behind in understanding how Alzheimer’s disease works and in developing ways to counter its progression. “We’re just now understanding some of the fundamental biology of it,” Grabowski says. He describes amyloid plaques and twisted strands of proteins—tangles—that are suspects in the death of nerve cells and the loss of brain tissue that come with Alzheimer’s. “There are too many suspects, and they all know each other,” he says. “It’s like ‘Murder on the Orient Express.’”
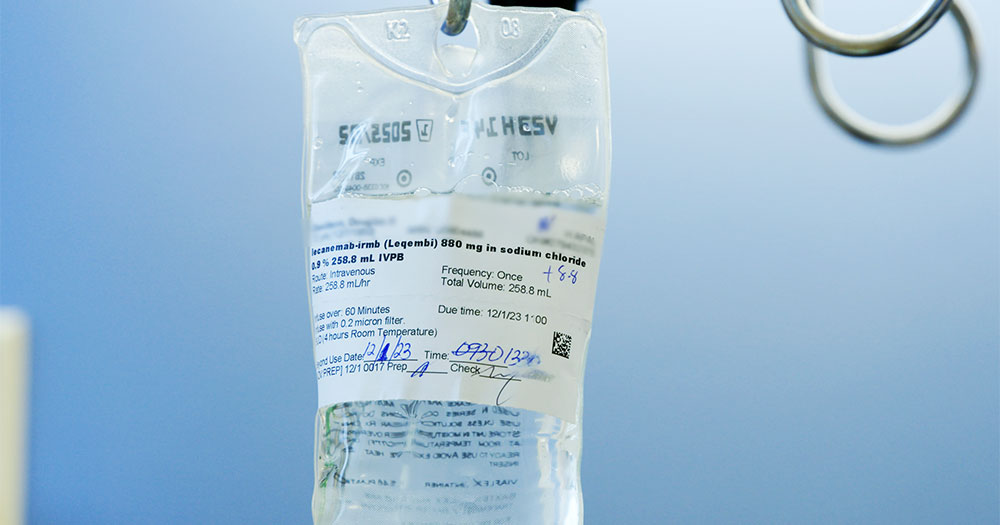
The intravenous solution of lecanemab prescribed for UW Medicine patient Doug Davidson. Photo by Randy Carnell / UW Medicine.
Until now, doctors have only been able to control some of the cognitive and behavioral symptoms of the disease. Enter the new drug lecanemab, which is shown to slow the progression of Alzheimer’s in patients in the early stages of the disease and to reduce the presence of amyloid plaques. An antibody, lecanemab binds to the plaques and stimulates the immune system to remove the amyloid. In testing, the drug slowed the patients’ rate of decline by 27% over 17 to 18 months. Of note, while most Alzheimer’s drug trials have lacked racial diversity, about 25% of the lecanemab trial participants were either Black or Hispanic; both populations are 1.5 times as likely as white individuals to develop the disease.
Last July, the Food and Drug Administration approved lecanemab, which is sold under the brand name Leqembi, for the treatment of Alzheimer’s disease. That same month, Dr. Michael Rosenbloom joined the UW Memory & Brain Wellness Center. One of his roles is to champion efforts to make the medicine available to patients. “It took six months to figure out what we needed in order to do it,” he says. The drug is administered through IV infusion every two weeks, and patients need regular MRI scans. While the benefits are described as modest, “it’s a new milestone in the treatment of Alzheimer’s disease,” Rosenbloom says.He describes the medicine as a major step forward. “It’s probably the beginning of a new order in how we treat Alzheimer’s.”